Intermittent fasting while breastfeeding — is it safe?

If you’re a new parent, firstly, you’re amazing. Your body has just gone through a superhero-level transformation, your bundle of joy has probably gifted you sleepless nights alongside the smiles, and you’re here, reading this article and doing due diligence with your health?!

We’re beyond impressed.
Now that you’ve given yourself a well-deserved high five, let’s get to it.
Maybe you’ve done intermittent fasting before and want to jump back in. Maybe you’re wondering if it could be a good way to boost energy levels or lose baby weight. Or maybe you’re simply looking for new opportunities to support that super strong postpartum body of yours — especially in its new role as caterer, personal assistant, and literal life force to a tiny human — and you want to learn more about intermittent fasting for beginners.
Whatever your reasons, we’ll cut to the chase: intermittent fasting while breastfeeding can be very unsafe for both you and your baby, and our experts don’t recommend it.
We’ll dig into the “why” as well as answer common questions like “Can you fast while breastfeeding?” and “Is intermittent fasting safe while breastfeeding?” but if the brain fog is creeping in, just remember, you should always speak with your healthcare provider if you’re thinking about fasting while breastfeeding.

Can you do intermittent fasting while breastfeeding — what does the research say?
You know how frustrated you get when you’re having an argument a discussion and the other person swears they’re right but can’t point to the proof?
Without those concrete, undeniable facts, it’s hard to advocate for something. And that’s exactly why we don’t recommend fasting while breastfeeding — there just isn’t evidence to support it’s a safe, health-promoting choice in any context, and what we do know is that it makes it even more challenging to meet your nutritional needs during this time.
Due to ethical and safety concerns, conducting experimental research with women and people who are pregnant or nursing is tricky, but the limited existing studies raise concerns that intermittent fasting may lead to a reduced supply of breast milk or alter its nutrient composition (so its macronutrients and micronutrients are out of whack).[1, 2,3]
These potential risks are likely due to the fact that intermittent fasting often involves eating fewer calories and a shorter eating window than usual, which means you’d need to put in extra effort to meet nutritional needs — and people who are breastfeeding already need to factor in additional calories and nutrition to support milk production. We’re just not prepared to risk any possible harm to you or your baby in what’s already a period when recovering and taking care of your baby is vital!
In other words, intermittent fasting may make it even more difficult for you and your baby to get everything your bodies need, especially when it comes to helping your baby grow and gain weight. And when it comes to the health and well-being of your baby, we know the biggest risk you’d want to take is burping them over that new sweater you just bought.
While we discourage fasting and breastfeeding together, we’re ready to stand in your corner and be your fasting support squad once you’ve finished breastfeeding. You can head over to our Simple quiz to learn about all the ways intermittent fasting may help keep you fit and fighting — for you and your child.
So, is it safe to intermittent fast while breastfeeding?
Okay, so can you intermittent fast while breastfeeding?
We don’t recommend intermittent fasting during breastfeeding for anyone. Let’s look at the reasons why.
Here’s what we know so far:
- New mothers and people who are breastfeeding need additional calories and nutrients to support milk production,[4] especially because their bodies are using up energy at a faster rate when lactating.
- Not getting enough calories or hydration may reduce the quality of the breast milk and make it harder to produce milk in the first place.
- Two of the most common intermittent fasting side effects include malnutrition and dehydration.
- In a few rare cases, fasting for more than 24 hours during lactation has been linked to a life-threatening condition called ketoacidosis.[5]
Logically, these four things stack up in what feels like a pretty precarious Jenga situation. It would take a lot of careful attention and deft planning to keep everything balanced if you were to fast during breastfeeding, and even then, it’s not guaranteed to be safe for you and your baby. Plus, certain types of fasting schedules (like water fasting, Eat Stop Eat, the 5:2 diet, alternate-day fasting, OMAD, and 20:4 intermittent fasting) significantly reduce calorie intake and the amount of time you have for eating, so it’s even harder to keep your tower of nutrients and hydration intact.
Still, while we strongly don’t recommend playing this particular game of risk, your healthcare provider may have a specific schedule in mind that they deem safe for you. If (and only if) you’ve got the green light, you can start intermittent fasting. However, you’ll still need to follow their instructions to a “T” to make sure you’re consistently and completely meeting your increased caloric, nutritional, and hydration needs.
Are there any health benefits?
Breastfeeding on its own has been linked to various physical health and mental health benefits for both the parent and the baby,[6,7] and intermittent fasting has also been associated with lots of positive health outcomes (like losing weight, supporting heart health, and promoting healthy brain aging, to name just a few).[8,9,10,11]
However, much like layering mini skirts over jeans, chunky belts over shirts, and shrugs over tank tops, “more” doesn’t always equal “better.”
When combined with intermittent fasting, breastfeeding benefits don’t necessarily compound (or vice versa). While there isn’t enough research on intermittent fasting while breastfeeding to say for sure whether there might be some benefits — and if so, to what extent and under what conditions — what we see so far is that if anything is compounded, it’s the potential risk. After giving birth, your priority is recovery, and fasting makes it harder and riskier for you to have a quick recovery.
When can I get back to intermittent fasting?
Other than sharing the traits of incredible strength and stamina, every postpartum body is different. What might be the ideal time for you to get back to intermittent fasting may not be right, safe, or effective for someone else.
It’s like what we say about fasting-based food routines in general: your body is your body, and the right approach is what’s best for you and your needs, goals, and lifestyle.
That’s one reason why it’s super important that you speak with your healthcare provider before beginning (or restarting) an intermittent fasting schedule: they’ll be best placed to help you figure out the what, when, and how of safe, effective fasting.
Regardless, we recommend resuming intermittent fasting once you’ve stopped breastfeeding completely. Like any routine that’s out of practice, though, you’ll want to ease into it — and that’s where we can help! You can take our Simple quiz to explore the different types of intermittent fasting schedules and how they might work for you. Regardless, the most important thing to remember is to start small, go slowly, and give yourself all the slack you need. Your body has just been through a lot!
Things to consider about your nutrition while breastfeeding

Brace yourselves for a Baby-Shark-level repetition moment: we don’t recommend intermittent fasting while breastfeeding unless you’ve already gotten that sweet medical approval. (And if that’s the case, your doctor will provide all the instructions and advice you need for a safe fasting experience.) However, in most cases, the advice will be the same: you can start fasting once you’ve finished breastfeeding completely.
Now that we’re crystal clear on that critical refrain, we do have some general nutrition advice for people who are breastfeeding.
(Also, apologies to anyone who now has Baby Shark stuck on a mental loop.)
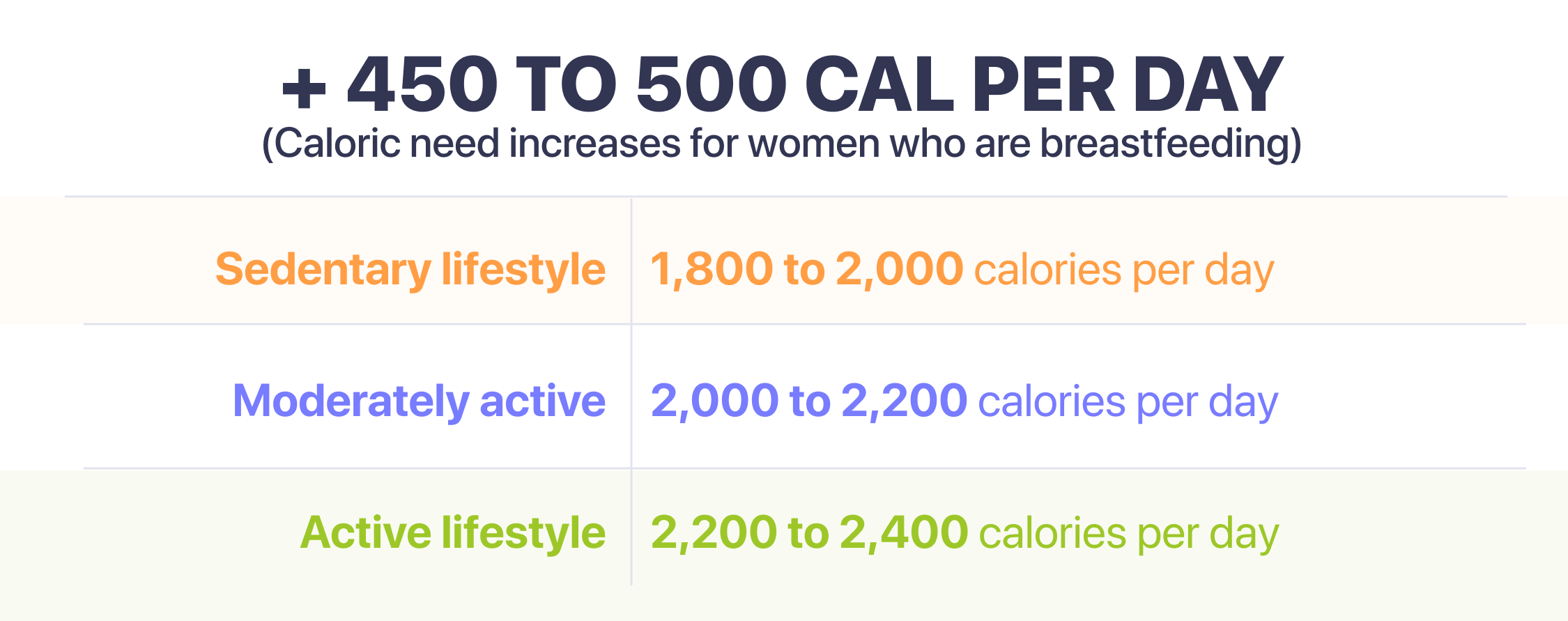
- Your caloric intake. You’ve heard of eating for two during pregnancy, and the same is true for breastfeeding. You need an eating routine that gives you adequate time and space to eat all the additional calories you need to support yourself and your baby. Typically, you need around 330–400 kcal more than your standard recommended intake, but you can also use this CDC-approved calculator to help you estimate your needs based on other factors like age, BMI, and activity levels.
- Your nutrient intake. Beyond needing more calories in general, you also need higher levels of iodine and choline during lactation. The Dietary Guidelines for Americans recommend 290 mcg of iodine (found in eggs, dairy, seafood, and iodized salt) and 550 mg of choline (found in dairy and protein like eggs, meats, beans, and lentils) daily. Likewise, particularly if you’re vegetarian or vegan, you may need additional support in reaching your recommended levels of vitamin B12, iron, zinc, and omega-3 fatty acids. Remember to also continue taking your postnatal vitamins daily or as otherwise instructed by your healthcare provider.
- Your seafood intake. While there aren’t any foods that are strictly off-limits to people who are breastfeeding, you want to be cautious about overdoing it on the seafood front since some fish contain high levels of mercury (which can impact your baby’s brain and nervous system). Eating a variety of fish from the “best” and “good” choices on the FDA chart is a good strategy, but you still want to monitor serving sizes (2–3 per week from the “best” category or 1 per week from the “good” category).
- Your hydration levels. People who are breastfeeding need around 2x as much water as the average person — so about 16 cups per day! If you’re getting sick of plain water, you can try adding fruit slices, herbs / spices, or a splash of juice for a flavor boost.
- Your caffeine intake. Caffeine can be passed in small amounts through breast milk. Low to moderate amounts of caffeine (the equivalent of 2–3 cups of coffee per day) should be fine, but if your baby is fussier or more sleepless than usual, it could be a sign that you need to rein in your caffeine consumption.
- Your meal times. With a newborn around, you may have already lost all sense of “normal” hours — whatever that means! — but now it’s time to get rid of any self-judgment around your meals. If you’re awake in the middle of the night and hungry for a midnight snack, don’t restrict yourself — it’s likely your body needs the fuel! Your current schedule is difficult enough to maintain and predict without trying to add arbitrary rules or standards to when you get the nutrition you need.
5 nutritional safety precautions you can take while breastfeeding
So, by now, you know breastfeeding and intermittent fasting aren’t a good mix. But what other nutrition-based safety precautions can you take while breastfeeding to ensure both you and your baby stay healthy and happy?
In addition to enlisting support from your household (this sh** is hard!) and having regular check-ins with your healthcare provider (it takes a village!), there are some action plans you can put in place to set you up for a safer breastfeeding experience.
1. Be on calorie patrol and prioritize nutrient-dense foods
In addition to making sure you’re meeting your daily calorie needs, you want to focus on eating foods that will fill you up with all the nutritional power-ups you and your baby need. Aim for a variety of fruits and leafy, green vegetables and sources of fiber, lean protein, and healthy high-fat foods.
2. Drink lots (and we mean lots) of fluids
Staying hydrated is always important and even more crucial when you’re already in a state where you need more H2O than ever before, so keep topping up that water bottle. Things like coffee, tea, and diet soda (one or two cans per day) are okay for hydration, too … but keep in mind that unless you’re reaching for those decaf options, you still want to be wary of caffeine content.
3. Keep a close eye on your baby’s growth and weight
When you’re breastfeeding, breast milk plays a fundamental role in your baby’s health and development.[12] If you have concerns about your baby’s growth, speak to your healthcare provider and make sure you and your baby get a thorough checkup to see what’s going on.
4. Minimize stress and maximize sleep
We know these concepts sound like an oxymoron (or a fantasy) to most new parents, but stress and sleep deprivation are associated with an increase in the production of cortisol,[13,14] which is a hormone that can cause lots of adverse physical and mental health effects (like high blood pressure, high blood sugar, and lack of focus) if your levels get too high. You never want your eating routine to be one that is causing you extra stress / anxiety or interfering with your sleep routine. If you feel that these two factors are bothering you, remember to speak with your healthcare provider — they really can help you.
5. Don’t channel the “no pain, no gain” mentality
When you’re breastfeeding, it’s extra important to listen to your body because it’s already working overtime to support you and your baby. Pushing it too hard or ignoring those hunger grumbles could be unsafe for you both. If your body’s sending you the signal that it’s not feeling quite right, it’s time to reconvene with your healthcare provider and reassess your strategies.
Are there any healthy alternatives to intermittent fasting while breastfeeding?

Let’s revisit what we said about the fashion era with layers on layers of clothing and accessories. Similar to the “more” doesn’t always equal “better” phenomenon, just because you can do something doesn’t mean you should.
So even if your healthcare provider told you “yes” when you asked them, “Can I fast while breastfeeding?” there may still be better ways to achieve your health goals with less risk.
For example, some studies suggest that people who are breastfeeding can continue regular and light-to-moderate physical activity without interfering with breast milk supply or quality.[15] Exercise during breastfeeding has also been linked to protection from bone density loss and reduced long-term, chronic health risks for the baby.[16,17]
It’s not like you have to be a marathon runner or CrossFit devotee to see those benefits, either; even something like walking or light stretching can massively boost your physical and mental health (and yes, support weight loss).[18] As with any type and level of physical activity, you just want to be cautious about overextending.
Likewise, focusing on specific lifestyle elements that have knock-on effects on areas of health and well-being may create a chain reaction of physical and mental improvements. Sleep is the obvious biggie here: it may be hard to come by with a newborn, but finding ways to soothe postpartum insomnia and manage odd waking hours can support everything from weight loss and improved gut health to better mental health and improved cognition in people who are not either pregnant or breastfeeding.[19,20,21,22] Limiting sources of caffeine (including chocolate!), practicing good sleep hygiene, and carving out even just a few minutes for a wind-down routine can go a long way in supercharging your sleep quality!
Yes, in some cases, fasting can decrease milk supply if you’re intermittent fasting while nursing. This reduction is likely due to a lack of nutrients and an unfavorable balance of macro- and micronutrient composition,[1,2] so it may also be more common in people undertaking consistent and longer fasts.
- Faris MAIE, Al-Holy MA. Implications of Ramadan intermittent fasting on maternal and fetal health and nutritional status: A review. Med J Nutrition Metab [Internet].
- Leiper JB, Molla AM, Molla AM. Effects on health of fluid restriction during fasting in Ramadan. Eur J Clin Nutr. 2003 Dec;57 Suppl 2:S30–8.
- Rakicioğlu N, Samur G, Topçu A, Topçu AA. The effect of Ramadan on maternal nutrition and composition of breast milk. Pediatr Int. 2006 Jun;48(3):278–83.
- CDC. Maternal diet [Internet]. Centers for Disease Control and Prevention. 2023 [cited 2023 Jun 12].
- Gleeson S, Mulroy E, Clarke DE. Lactation Ketoacidosis: An Unusual Entity and a Review of the Literature. Perm J. 2016 Feb 22;20(2):71–3.
- Sen S. Breast Milk and Breastfeeding: Benefits, Barriers, Maternal Predictors, and Opportunities for Innovation. Clin Ther. 2022 Feb;44(2):170–1.
- Tucker Z, O’Malley C. Mental Health Benefits of Breastfeeding: A Literature Review. Cureus. 2022 Sep;14(9):e29199.
- Abeyasekera KN. Benefits of Intermittent Fasting: A Systematic Review of Randomized Clinical Trials. 2020.
- Varady KA, Cienfuegos S, Ezpeleta M, Gabel K. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol. 2022 May;18(5):309–21.
- Yang F, Liu C, Liu X, Pan X, Li X, Tian L, et al. Effect of Epidemic Intermittent Fasting on Cardiometabolic Risk Factors: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front Nutr. 2021 Oct 18;8:669325.
- Francis N, George & Anne Ryan Institute for Neuroscience, University of Rhode Island, 130 Flagg Road, Kingston, RI, 02881, US, Department of Psychology, Stony Brook University, 100 Nicolls Rd, Stony Brook, NY, 11794, US. Intermittent fasting and brain health: Efficacy and potential mechanisms of action. OBM Geriatrics. 2020 Jun 1;4(2):1–19.
- Martin CR, Ling PR, Blackburn GL. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients [Internet]. 2016 May 11;8(5).
- James KA, Stromin JI, Steenkamp N, Combrinck MI. Understanding the relationships between physiological and psychosocial stress, cortisol and cognition. Front Endocrinol. 2023 Mar 6;14:1085950.
- Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: From physiological to pathological conditions. Sleep Sci. 2015 Nov;8(3):143–52.
- McRoy J. The effects of exercise on breastmilk composition and supply: A critical literature review [Internet]. James Madison University; 2020.
- Lee LL, Huang SF, Lai PC, Huang YT. Effect of exercise on slowing breastfeeding-induced bone loss: A meta-analysis and trial sequential analysis. J Obstet Gynaecol Res. 2020 Sep;46(9):1790–800.
- Harris JE, Pinckard KM, Wright KR, Baer LA, Arts PJ, Abay E, et al. Exercise-induced 3’-sialyllactose in breast milk is a critical mediator to improve metabolic health and cardiac function in mouse offspring. Nat Metab. 2020 Aug;2(8):678–87.
- Kołomańska-Bogucka D, Mazur-Bialy AI. Physical Activity and the Occurrence of Postnatal Depression-A Systematic Review. Medicina [Internet]. 2019 Sep 2;55(9).
- Papatriantafyllou E, Efthymiou D, Zoumbaneas E, Popescu CA, Vassilopoulou E. Sleep Deprivation: Effects on Weight Loss and Weight Loss Maintenance. Nutrients [Internet]. 2022 Apr 8;14(8).
- Smith RP, Easson C, Lyle SM, Kapoor R, Donnelly CP, Davidson EJ, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019 Oct 7;14(10):e0222394.
- Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. 2021 Dec;60:101556.
- Mantua J, Simonelli G. Sleep duration and cognition: is there an ideal amount? Sleep [Internet]. 2019 Mar 1;42(3).
