Intermittent fasting and diarrhea — explained by Simple

Picture it: you’ve just started intermittent fasting. You’ve picked your approach, you’ve got a meal plan ready to go, and your motivation is sky-high.
After a successful first fasting window, you sit down, do a little celebration shimmy, and dive into your eating window with gusto.
And then you find yourself running to the toilet.

Sounds like a pretty crappy situation.
(Yep, we’re going to plunge right into the toilet puns here.)
While diarrhea is a totally normal phenomenon that most of us occasionally experience, during intermittent fasting, diarrhea can be a sign that something is off, especially if it persists and is not something you’re used to on the reg. Fasting diarrhea can also be dangerous since it can exacerbate other potential intermittent fasting side effects, like dehydration and malnutrition.
But before you start flushing those fasting plans down the drain, let’s make sure we’re on the same page about diarrhea and fasting and clear up common questions like “Does fasting cause diarrhea?”
If you need a quick pit stop to remember what intermittent fasting is in the first place, you can also check out our guide on intermittent fasting for beginners.

Experiencing diarrhea while fasting — is it normal?
Diarrhea occurs when not enough water has been removed from your stool or too much fluid is secreted into your stool. Lots of things can cause it, but basically, it’s when things are rushing through your system.
Now the concept of “having the runs” probably makes even more sense … diarrhea is like everything is fleeing your body without being digested properly. If diarrhea becomes a chronic issue, it can leave you at risk of developing various nutritional deficiencies along the way, which is why keeping an eye on your stool is essential for good health.
While it’s common for many of us to experience diarrhea from time to time, it’s not usually normal to have diarrhea during fasting windows since you don’t have food entering your digestive tract. However, it can be triggered by the process of breaking your fast. We’ll go into the specifics of “how” in the next section.
As a bottom line, it’s worth keeping in mind that the occasional bout of diarrhea during the intermittent fasting process isn’t typically something to raise the alarm about — but since diarrhea can be acute or chronic, it is a sign that you may need to take a closer look at your eating habits and general lifestyle and make some adjustments. It’s also not something that’s normal to experience consistently, either, so if you find yourself spending lots of time scrolling through TikTok from the bathroom, it’s time to speak with your primary care provider.
Whether you’re experiencing intermittent fasting side effects, looking to avoid intermittent fasting mistakes, or just have questions about what to expect from the general fasting process (like “Does intermittent fasting slow your metabolism?”), we’re here to help you get the answers you need to make the right decisions for you and your body. While we’re not a replacement for a medical team — and you should always consult them before making any significant eating routine changes — you can take our Simple quiz to learn more about intermittent fasting schedules, get insight into the process, and see how it might affect you.
What can cause diarrhea during intermittent fasting

If the thought of “having the runs” has you wanting to run away from fasting, let’s get one thing straight: fasting doesn’t inherently cause diarrhea. In fact, there currently is little to no data linking both together.
So, why does intermittent fasting cause diarrhea in some cases? Well, it’s not so much “cause” as it is “facilitate the potential.”
When you’re fasting, you’re not sending any external nutrients into your digestive tract. That means your digestion process shifts to focus on absorbing what you’ve already consumed and turning that into useful body stuff, like energy, muscle, and brain power. It also means your bowels are just chilling, enjoying a break from separating nutrients and waste.
But you know that feeling of returning from vacation, seeing thousands of emails, and feeling even more stressed by work than you were before you left?
The same thing can happen to your bowels when you break your fast. Since your bowels are now more sensitive — they haven’t had to work in a while — they can easily be overwhelmed if you make them work extra hard at the start of your eating window. Going too long between meals is actually similar to how your body reacts to anxiety: it releases a stress response, which can impact the digestive system, which in turn can mean … bathroom trips galore.
So, while intermittent fasting may actually benefit your digestion overall by improving the balance of your gut bacteria and reducing inflammation associated with some tummy troubles,[1,2] it (like any change to your eating habits) can also cause digestive system disruptions, like diarrhea, constipation, bloating, and nausea. It also may just take some getting used to.
If you’ve experienced diarrhea after breaking fast, it may be worth evaluating your eating routine to see if there are any potential triggers. For example, the following things may create extra stress for your bowels:
- Fried, greasy, and/or fatty foods. Foods like chips and fried chicken, especially when eaten in excess, encourage muscle contractions and can mess with how your body processes fat,[3] both of which can lead to diarrhea.
- Sugar alcohols. If you’re trying to cut back on calories to lose weight, you may be eating more sugar alcohols. Not to be confused with actual alcohol, these sugar-like substances are often found in sugar-free foods like sweets, drinks, and gum. These sweeteners can irritate your digestive system and leave you more prone to diarrhea.[4]
- Caffeine. Having more caffeinated drinks (like coffee, green tea, and soda) could likewise lead to diarrhea, as caffeine acts as a stimulant for your digestive system. People with IBS or living with overweight or obesity may be especially sensitive to these caffeine boosts.[5]
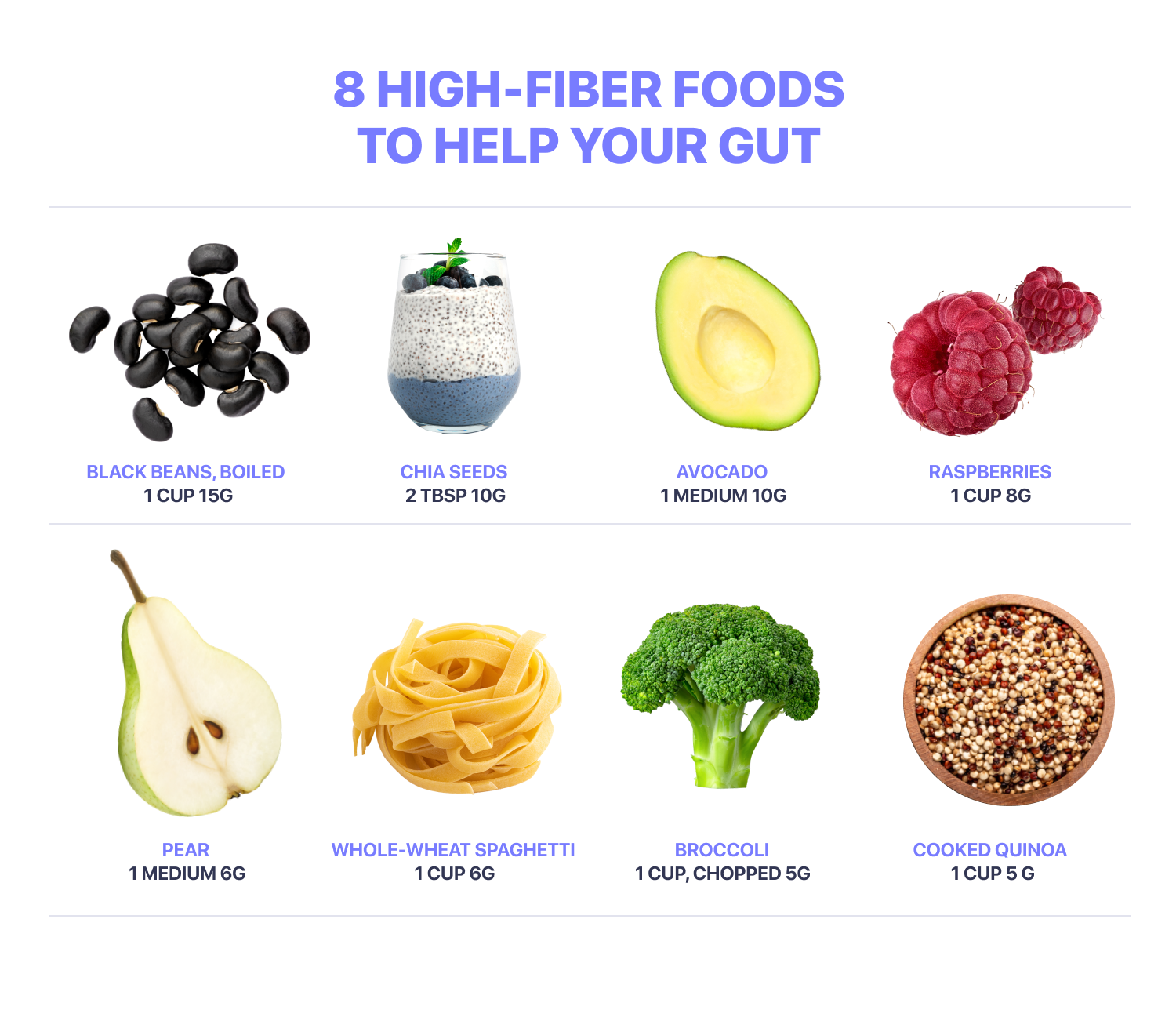
- Too little fiber. Fiber is a form of carbohydrate most commonly found in plant-based foods (like fruits, vegetables, and whole grains). It can’t be broken down in your body and instead is fermented in your colon, which is why it plays a crucial role in keeping your gut healthy. If you’re not used to consuming adequate amounts of it daily, getting too little fiber may be triggering your diarrhea. Try to increase your intake gradually and start off with foods rich in soluble fiber (which can help increase water retention in your gut and reduce loose stools). Aim for foods like oats, bananas, bran, or barley.
- Too much fiber. They really weren’t lying when they said moderation is key! While getting enough fiber is important, for some people, having too much of the stuff may also be an issue. That’s why we always recommend gradually increasing your fiber intake — particularly with those fiber-rich foods that are more fermentable, which can draw more water into the colon and increase your risk of diarrhea. Easy does it with things like mangoes, dates, apples, legumes, leafy veggies, onions, and garlic, so you can test your boundaries without leaping way beyond them.
- Lactose or capsicum intake. If you’re normally sensitive to capsicum or lactose, which can trigger diarrhea even without fasting, your stomach may be extra sensitive to these ingredients after fasting.
- Large meals. If you have a short eating window, you may find yourself gravitating towards less frequent, larger meals to meet your nutritional needs. Having larger meals can put stress on the gut, which may, in turn, trigger diarrhea. Try breaking these meals up into smaller, more frequent meals and snacks.
- Getting overly hungry. Hunger is common when starting to fast or trying a longer fasting schedule, but if you get to a point where you’re ravenously hungry, you may be more likely to binge, eat too quickly, or choose less health-promoting foods — all of which may increase your likelihood of diarrhea. If this situation sounds all too relatable, you could always try having a meal ready to eat when your fast ends or even try scaling your fasting window back a little until your hunger cues adjust.
While fasting and diarrhea don’t necessarily have a causal link, some general causes of diarrhea can also overlap with the fasting process. For example, mineral deficiencies can cause diarrhea,[6] and having a shorter eating window may mean you find it harder to get all the nutrients you need for the day. Similarly, stress levels and certain medications, exercise routines / workout timings, and underlying medical conditions can make you more sensitive to diarrhea, so it’s important to speak with your doctor before fasting if you’re already at risk for diarrhea and are considering fasting.
Common side effects of diarrhea while fasting
Our bodies are uniquely beautiful things, and as slightly weird as it may sound, that goes for our bowel movements, too. What’s “normal” for our body may not be “normal” for someone else, and that’s also true for if, how, and to what extent we experience diarrhea during intermittent fasting.
The challenge when it comes to intermittent fasting and diarrhea is that any type, level, or amount of diarrhea can exacerbate and compound the potential side effects fasting already brings to the table. These side effects can include:
- dehydration
- cramping
- bloating
- headaches
- nausea
- dizziness / lightheadedness
- fatigue
- malnutrition
- malabsorption
- fainting
While most of these side effects can be easily resolved by breaking your fast, rehydrating, replenishing lost electrolytes through rehydration salts, and/or reevaluating your diet and eating habits, experiencing any number two side effects is a sign you need to keep a closer eye on number one — and by that, we mean you. If any of these symptoms persist beyond a week or are severe, you should consult your healthcare provider before continuing your fasting schedule.
5 tips on how to prevent diarrhea during intermittent fasting
Ready to flush that diarrhea straight out of your fasting experience?
(Yep, we’ll continue clogging this article with these sorts of crappy, cringey puns.)
Even though everyone’s experiences with intermittent fasting differ, there are some tricks that can help you — and your bowels — be safe and comfortable.
You might even say that you both can then … focus on the good sh**.
1. Reduce fatty foods, caffeine, and sugar alcohols
Limiting those digestive irritants we mentioned earlier is a great way to limit your chances of having diarrhea after breaking your fast. If you are breaking your fast thanks to diarrhea, you may also consider foods that are easier to digest and known to alleviate your symptoms, like bananas, rice, applesauce, and toast.
2. Gradually introduce more fiber into your eating routine
Soluble fiber (stuff that draws water into the gut) and insoluble fiber (stuff that helps food pass more quickly through the stomach and intestines) are both helpful for your general metabolic health and supporting regular bowel movements,[7] but the soluble stuff is particularly good for fending off diarrhea and dehydration.
There are plenty of foods high in soluble fiber that you can try — like black beans, sweet potatoes, avocados, oats, fruits, and sunflower seeds — but just make sure you start small and ease into it so you don’t overwhelm your bowels in a fiber flood. Some people may also be more sensitive to fiber, so if you start feeling bloated, crampy, or tooty, you may have gone too far. You can also check out our general guide on what to eat during intermittent fasting for more food-related tips and meal-planning advice.
3. Eat smaller meals more often
Remember the work email analogy? It’s a lot easier to get overwhelmed and have things slip through the cracks — perhaps an unintentionally crude word choice here — if you throw a lot at your system all at once. Eating smaller, more frequent meals may give your digestive tract more of a chance to absorb what you send into it.[3] You can also take our Simple quiz to get an idea of what fasting vs. eating window structure might be your best fit.
4. Prioritize (re)hydration
Think of electrolytes and water as the superhero duo that can protect your body against the villainous diarrhea — and provide a lot of benefits in general since they help your body with essential things like pH balance, muscle contraction, and hydration. If you’re fasting, you can try a little salt in your water, or during your eating windows, you can sip coconut water, milk, fruit juice, Pedialyte, or other electrolyte solutions. Not sure what and when you can drink during intermittent fasting? You can read our guides on what you can drink while fasting and what breaks a fast.
5. Protect that mental health
Your gut and your brain are total empath BFFs — what affects one can directly affect the other through what’s called the gut-brain axis.[8] If you’re stressed, whether in general or because of the fasting experience, this stress can trigger changes to your bathroom experience. Managing your stress and mental health is always important for your health and well-being, but it’s especially crucial to fortify that self-compassion and self-care when you’re making changes to your routine that could add extra challenges to your day.
If you’ve experienced diarrhea while fasting and you’re raring to go on the troubleshooting, we recommend only trying one thing from this list at a time. That way, you’re more likely to learn what works rather than throw everything at it and not know what’s actually most effective.
Other reasons why you should stop your fast
While most intermittent fasting side effects are mild and short-lived, we’re big advocates of knowing thyself: if your body is sending messages that something isn’t right, don’t leave yourself on read. Especially if you’re having persistent or severe side effects, pay attention to those notifications.
You should also be particularly quick to stop fasting if you experience
- chest pain
- general abdominal pain
- nausea / vomiting
- dizziness / vertigo
- fainting / loss of consciousness
- persistent fatigue
- fever
Even if something just feels off, but you can’t put your finger on what, keep checking in with yourself — whatever you’re feeling may be the first sign of a reason to stop fasting.
When should you go see a doctor?
If your diarrhea doesn’t resolve itself relatively quickly, it’s time to speak to a healthcare professional. This timing is especially crucial if diarrhea is a longstanding issue for you (and may not be specifically fasting-related).
You should also consult your healthcare provider if you experience any pain during bowel movements or spot any grease, changes in color, or blood / mucus in your stool. These could be warning signs of a more serious issue.
Our bottom line when it comes to your health and well-being is that it’s never worth a risk. Even if you haven’t experienced these specific situations, but something doesn’t feel right, or you’re deep in the “intermittent fasting not working” frustration, don’t be afraid to speak with your primary care provider.
Frequently asked questions about intermittent fasting and diarrhea
If you have disordered electrolyte transport (often caused by infection or digestive disorders) that leads to secretory diarrhea, it does typically persist during fasting.[9] We recommend speaking with your doctor before beginning any fasting schedule if you have irregular digestion or other chronic medical conditions.
- Hu D, Xie Z, Ye Y, Bahijri S, Chen M. The beneficial effects of intermittent fasting: an update on mechanism, and the role of circadian rhythm and gut microbiota. Hepatobiliary Surg Nutr. 2020 Oct;9(5):597–602.
- Wang X, Yang Q, Liao Q, Li M, Zhang P, Santos HO, et al. Effects of intermittent fasting diets on plasma concentrations of inflammatory biomarkers: A systematic review and meta-analysis of randomized controlled trials. Nutrition. 2020 Aug 12;79-80:110974.
- O’Brien L, Wall CL, Wilkinson TJ, Gearry RB. What Are the Pearls and Pitfalls of the Dietary Management for Chronic Diarrhoea? Nutrients [Internet]. 2021 Apr 21;13(5).
- Mäkinen KK. Gastrointestinal Disturbances Associated with the Consumption of Sugar Alcohols with Special Consideration of Xylitol: Scientific Review and Instructions for Dentists and Other Health-Care Professionals. Int J Dent. 2016 Oct 20;2016:5967907.
- Koochakpoor G, Salari-Moghaddam A, Keshteli AH, Esmaillzadeh A, Adibi P. Association of Coffee and Caffeine Intake With Irritable Bowel Syndrome in Adults. Front Nutr. 2021 Jun 15;8:632469.
- Semrad CE. Approach to the Patient with Diarrhea and Malabsorption. Goldman’s Cecil Medicine. 2012;895.
- Barber TM, Kabisch S, Pfeiffer AFH, Weickert MO. The Health Benefits of Dietary Fibre. Nutrients [Internet]. 2020 Oct 21;12(10).
- Barrio C, Arias-Sánchez S, Martín-Monzón I. The gut microbiota-brain axis, psychobiotics and its influence on brain and behaviour: A systematic review. Psychoneuroendocrinology. 2022 Mar;137:105640.
- Sweetser S. Evaluating the patient with diarrhea: a case-based approach. Mayo Clin Proc. 2012 Jun;87(6):596–602.
