Simple’s guide on intermittent fasting and blood sugar

Somewhere along the way, carbohydrates (think bread, pasta, potatoes, and rice) became the villains of the nutrition world. We don’t see them that way at Simple, however. The truth is that our bodies need carbohydrates — it’s the best energy source we’ve got.

Where we can get into difficulties is when we eat too many carbohydrates and simple sugars (like honey and sweets); don’t eat enough protein (such as chicken, fish, or tofu), healthy fats (like avocado or olive oil), or fruits and vegetables; and don’t move our bodies enough during our daily lives.
This can all lead to chronically elevated blood sugar,[1] and that’s a problem. Blood sugar is supposed to rise after you eat — this is perfectly normal — but it’s supposed to also go back down to a reasonable level. When it goes up and stays up, over time, this can lead to unwanted weight gain, heart disease, high blood pressure, prediabetes, and, in some cases, develop into type 2 diabetes.[2]
Let’s dive into all things blood sugar and see how intermittent fasting can help with blood sugar control.
What is blood sugar, and how does it work?
When you eat, your body breaks down most foods into glucose (the sugar found in our blood). Glucose is the body’s most important and preferred fuel source.
When glucose hits your bloodstream, the pancreas releases the hormone insulin. Insulin transports glucose into the cells to be used for energy.
Recently, there has been a lot of attention on blood sugars and wearing monitors to track how food can influence your levels. While it can seem appealing to have this knowledge, there is a lack of data available to back up any additional benefits of tracking your blood sugars in healthy individuals without diabetes.
If we eat too many carbohydrates and/or don’t pair them with the other macronutrients, we end up with a rapid blood sugar spike, and our bodies release even more insulin to try to get it back under control. If there’s too much sugar or our cells can’t accept it (a sign of insulin resistance), our bodies store the excess glucose as fat. This can lead to weight gain, obesity, and the development of chronic diseases like diabetes, high blood pressure, heart disease, and some cancers.
Does intermittent fasting lower blood sugar?
Before we get into the benefits of intermittent fasting (they extend far beyond weight loss!), let’s talk about what intermittent fasting is.
Intermittent fasting is time-restricted eating (TRE) — a way to reduce the number of calories you eat by limiting eating to a certain time window instead of counting calories or cutting out food groups.
One of the most popular TRE fasting schedules is 16:8, where you fast for 16 hours and eat during an 8-hour window every day. 16:8 is an effective schedule, but there are lots of variations — like 12:12, 14:10, 18:6, and alternate day fasting (which we at Simple don’t recommend over our fav TRE) — that you can choose to fit your lifestyle. Intermittent fasting for beginners can be a little tricky, so if you need some extra support, take our Simple quiz, and we’ll help you get started.
OK, back to the benefits. How does intermittent fasting affect blood sugar?
Intermittent fasting has been shown to lower blood sugar and cholesterol, which may help reduce your risk for type 2 diabetes and heart disease.[3] It has also been shown to increase your resistance to stress and suppress inflammation.[4]
It’s important to know, too, that to hold onto any blood sugar benefits, you’ll need to stick with fasting for the long haul. Improvements in blood sugar that come from fasting depend on how long you’ve stuck to your intermittent fasting schedule. As the famous saying goes, Rome wasn’t built in a day, right? If you stop, fasting’s positive impact on your blood sugar regulation will also stop unless you can find an alternative arrangement to sticking to a balanced diet and a healthy lifestyle.
When fasting, especially over the long term, listening to your body is key. Notice any intermittent side effects you may be experiencing, and remember it’s OK to take a break or change up your fasting schedule as your needs and goals change. You can always check back in with us for some guidance (the Simple app is made for this!), and regular check-ins with your doctor are a good idea, too.
Studies on blood sugar and fasting
More and more research is being done on intermittent fasting and its possible health benefits, but not all studies show that it’s the final answer to lowering your blood sugar levels.
Some research on healthy men carrying extra weight suggests that daily calorie restriction and diets that mimic fasting also positively affect blood glucose levels.[5] Is it just plain old calorie restriction that reduces fasting glucose levels?[6]
Even if that is true, intermittent fasting is a way to achieve that calorie restriction that many people find easier to manage. Limiting your calories using the clock rather than a calorie counter can really lighten the mental load.
While many studies connect intermittent fasting to stress reduction,[7] more research is needed to explore the links between how both are linked together fully, but these results are exciting nonetheless. If you feel like stress could be a reason that intermittent fasting may not be working for you, check in with your doctor. Reevaluate your fasting schedule and look for possible intermittent fasting mistakes that may be getting in your way.
Fluctuating blood glucose levels can also increase oxidative stress.[8] This is one reason why knowing what to eat during intermittent fasting is crucial. Eating more foods high in lean protein, healthy fats, and fiber can help you avoid that blood sugar yo-yo effect.
If you need a hand knowing what to eat for great health or getting intermittent fasting to work for you, take our Simple quiz and set up your free account on the Simple app. We’ve got the tools (like fasting reminders and food trackers) and resources (like feedback on your meals and expert articles) you need to kickstart your progress.
How does intermittent fasting affect blood sugar levels?
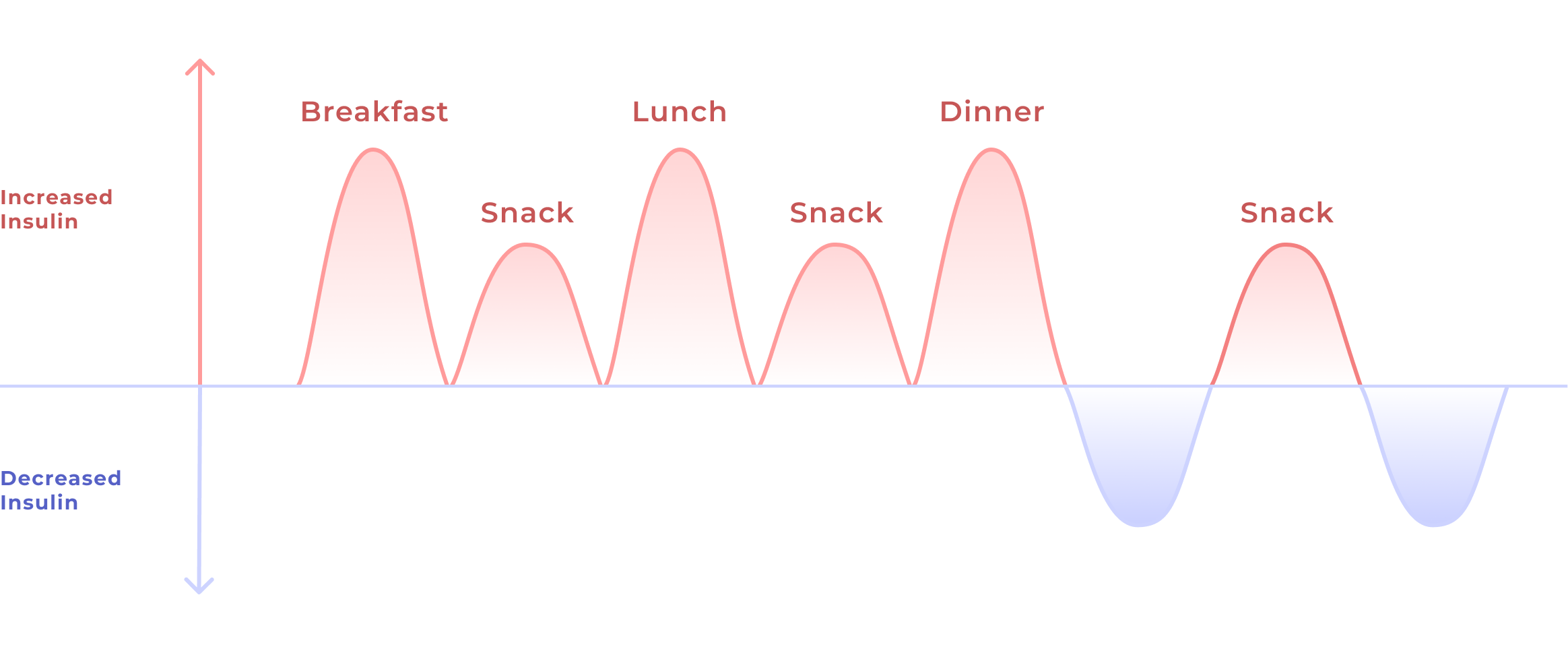
When you eat, your metabolism kicks in, and the body releases insulin. Insulin is a major player in how your body uses and stores energy.[9] The carbohydrates in the food we eat are broken down into glucose in the bloodstream. Insulin acts as a key to unlock and open the cells to absorb that glucose to either use as energy or — if there’s excess — to store as fat.
Intermittent fasting has been shown to flip a metabolic switch, changing the signaling pathways.[10] Fasting reduces insulin levels because there is no glucose to process, and the body is forced to tap into fat stores for energy. With more and more research behind it,[11] this “switch” is pushing intermittent fasting for diabetes to the top of therapeutic options.
Who should avoid intermittent fasting?
We always recommend that anyone who’s interested in intermittent fasting check with their doctor before getting started. This is especially true if you are someone who:
- is pregnant, breastfeeding, or trying to conceive
- has type 1 diabetes
- is on prescription medications
- is under 18 years old, or 80 years old or more
- is extremely active
- has a body mass index (BMI) < 18.5
- has an eating disorder or a history of one (or is at risk of developing one)
If you fall into one of these categories and still decide to try fasting, keep your doctor involved from start to finish.
How to control blood sugar with intermittent fasting

If you’d like to try intermittent fasting for blood sugar control, there are a few things to consider, especially if you have type 2 diabetes. These six tips will help support you as you start intermittent fasting for lower blood sugar levels:
1. Choose an intermittent fasting schedule that won’t cause you stress
On fasting days, your insulin levels decrease. In response, your body releases hormones from your liver, one of which is cortisol, a stress hormone. Cortisol tells the liver to release more glucose.[12]
If you do have diabetes, check your blood sugar regularly while fasting and keep your doctor informed of any changes you see. You may also want to consider working with a therapist for stress management because whether you’re fasting or not, stress may hinder your blood sugar control.[13]
Occasionally, although not the norm, intermittent fasting can cause low blood sugar (aka hypoglycemia).[14] If you have diabetes, this can potentially be dangerous since some diabetes medication already puts you at risk for low blood sugar. We can’t stress enough how important it is to keep your doctor informed of your plans to try intermittent fasting, especially if you’re on diabetes medications. It is possible for you to fast safely, but your doctor may need to make some medication adjustments to keep you safe and provide you with ongoing supervision.
Intermittent fasting can improve your insulin sensitivity and decrease your overall glucose levels.[3] These findings are promising, as healthy blood sugar regulation is vital in reducing your risk of cardiovascular disease and diabetes and for long-term health.
2. Stay hydrated
Hydration is important for blood sugar control whether or not you’re fasting. Know what you can drink while fasting to prevent dehydration and keep your insulin response and blood sugar low.
3. Eat well-balanced meals
During your eating window, try to include high-fiber carbohydrates like whole grains, fruits, and veggies; lean proteins such as lean meats, beans, and legumes; and healthy fats like avocados, fatty fish, nuts and seeds.
4. Get good quality sleep
Seven to eight hours of quality sleep are the magic numbers for overall wellness (though what’s ideal for you may vary). Sleep deprivation can increase insulin resistance, blood sugar levels, and food cravings, making it harder to stick to a fasting schedule.[15]
5. Exercise daily
Movement helps improve blood sugar control and insulin response [16] and is a great way to reduce stress,[17] especially if you’re moving in a way that you enjoy. It can also help you sleep better.[18] Fasting and exercise make a dynamic duo for maintaining healthy blood sugar levels.
6. Try early time-restricted eating (TRE)
Some research has shown early TRE — i.e., eating earlier in the day and starting your fast earlier in the evening — optimizes the metabolic circadian rhythms (the natural fluctuations of metabolic hormones) in men with prediabetes.[19] More research needs to be done on the importance of timing with intermittent fasting schedules for blood sugar, but you could always try early TRE for yourself and see how it helps you.
Frequently asked questions about intermittent fasting and blood sugar
How long before intermittent fasting lowers your blood sugar is typically around 8–12 weeks if you’re consistent with your fasts.[11] But everyone is different. Physical activity and what you eat during your fasting window will play a role in how quickly your blood sugar control can improve.
Normal fasting blood sugar levels range between 70 and 100 mg/dl for those without a diabetes diagnosis. If fasting blood glucose levels range between 100 and 125 mg/dl, this may indicate the beginning stages of glucose intolerance.[20] If you’re seeing these kinds of fasting glucose numbers, chances are your doctor will begin to closely monitor your blood sugar, and it may be a good time to chat with them about intermittent fasting.

- Good to Know: Factors Affecting Blood Glucose. Clin Diabetes. 2018 Apr;36(2):202.
- Ibrahim MS, Pang D, Randhawa G, Pappas Y. Risk models and scores for metabolic syndrome: systematic review protocol. BMJ Open. 2019 Sep 27;9(9):e027326.
- Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, et al. Effect of Intermittent Fasting Diet on Glucose and Lipid Metabolism and Insulin Resistance in Patients with Impaired Glucose and Lipid Metabolism: A Systematic Review and Meta-Analysis. Int J Endocrinol. 2022 Mar 24;2022:6999907.
- Wang C, Liu Z, Cai J, Xu X. The regulatory effect of intermittent fasting on inflammasome activation in health and disease. Nutr Rev [Internet]. 2023 Aug 27.
- Trepanowski JF, Kroeger CM, Barnosky A, Klempel MC, Bhutani S, Hoddy KK, et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern Med. 2017 Jul 1;177(7):930–8.
- Kim JY. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J Obes Metab Syndr. 2021 Mar 30;30(1):20–31.
- Berthelot E, Etchecopar-Etchart D, Thellier D, Lancon C, Boyer L, Fond G. Fasting Interventions for Stress, Anxiety and Depressive Symptoms: A Systematic Review and Meta-Analysis. Nutrients [Internet]. 2021 Nov 5;13(11).
- Wright E Jr, Scism-Bacon JL, Glass LC. Oxidative stress in type 2 diabetes: the role of fasting and postprandial glycaemia. Int J Clin Pract. 2006 Mar;60(3):308–14.
- Rahman MS, Hossain KS, Das S, Kundu S, Adegoke EO, Rahman MA, et al. Role of Insulin in Health and Disease: An Update. Int J Mol Sci [Internet]. 2021 Jun 15;22(12).
- Anton SD, Moehl K, Donahoo WT, Marosi K, Lee SA, Mainous AG 3rd, et al. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity . 2018 Feb;26(2):254–68.
- Barnosky AR, Hoddy KK, Unterman TG, Varady KA. Intermittent fasting vs daily calorie restriction for type 2 diabetes prevention: a review of human findings. Transl Res. 2014 Oct;164(4):302–11.
- Thau L, Gandhi J, Sharma S. Physiology, Cortisol. StatPearls Publishing; 2023.
- Sharma K, Akre S, Chakole S, Wanjari MB. Stress-Induced Diabetes: A Review. Cureus. 2022 Sep;14(9):e29142.
- Hypoglycemia rate “lower-than-expected” with intermittent fasting diet [Internet]. diabetes.medicinematters.com. 2018 [cited 2023 Nov 29].
- Daza EJ, Wac K, Oppezzo M. Effects of Sleep Deprivation on Blood Glucose, Food Cravings, and Affect in a Non-Diabetic: An N-of-1 Randomized Pilot Study. Healthcare (Basel) [Internet]. 2019 Dec 25;8(1).
- Bird SR, Hawley JA. Update on the effects of physical activity on insulin sensitivity in humans. BMJ Open Sport Exerc Med. 2016;2(1):e000143.
- Mücke M, Ludyga S, Colledge F, Gerber M. Influence of Regular Physical Activity and Fitness on Stress Reactivity as Measured with the Trier Social Stress Test Protocol: A Systematic Review. Sports Med. 2018 Nov;48(11):2607–22.
- Banno M, Harada Y, Taniguchi M, Tobita R, Tsujimoto H, Tsujimoto Y, et al. Exercise can improve sleep quality: a systematic review and meta-analysis. PeerJ. 2018 Jul 11;6:e5172.
- Sutton EF, Beyl R, Early KS, Cefalu WT, Ravussin E, Peterson CM. Early Time-Restricted Feeding Improves Insulin Sensitivity, Blood Pressure, and Oxidative Stress Even without Weight Loss in Men with Prediabetes. Cell Metab. 2018 Jun 5;27(6):1212–21.e3.
- CDC. Diabetes tests [Internet]. Centers for Disease Control and Prevention. 2023 [cited 2023 Nov 29].
