Intermittent fasting and diabetes — do they work together?

If you’re someone living with diabetes, chances are you’ve experienced fasting ahead of a blood test. But not all fasting is created equal.
Intermittent fasting involves a regular routine of timed eating windows and eating breaks. While the specifics and timing of this routine can vary, all intermittent fasting protocols focus on when you eat rather than what you eat.

As far as food routines go, it’s a pretty versatile choose-your-own-adventure — it’s light on rules and restrictions. You can tailor it to fit you and your needs, and it can lead to a whole host of potential benefits, like reduced inflammation and improved heart and brain health.
But that’s not even the best part: research shows intermittent fasting may be helpful in supporting the management and treatment of — and for some people, maybe even the remission of — type 2 diabetes.[1,2]
How? Why? For whom? Also … what even is intermittent fasting, exactly?!
Don’t worry, we’re not going to make you play amateur detective and create a true-crime-level research board of facts and theories. If you’re wondering whether intermittent fasting for diabetes is safe and effective — and if so, for whom and in what conditions — you’ve come to the right place.
Before we dive in, one quick note about fasting and diabetes if you’re in a TL;DR mood: people living with pre-, type 1, or type 2 diabetes should always get approval from their healthcare provider before starting any form of intermittent fasting, especially if they have any other health conditions. So, hold your horses (er, your fasting plans), and don’t rush through that starting gate until you’ve gotten the official green light!

Key takeaways
- Intermittent fasting and diabetes: like a blind date, sparks safely fly for some, but it’s definitely not a match made in heaven for everyone.
- For some people, it can be a useful way to lose weight, balance blood sugar levels, reduce inflammation, and improve insulin sensitivity. Plus, it can also decrease the chances of developing type 2 diabetes, help manage symptoms, or even put it in remission.
- Intermittent fasting can have an impact on folks with diabetes who use insulin or take medications for low blood sugar because it can cause their blood sugar levels to swing up and down, putting them at risk for hypoglycemia and hyperglycemia when fasting.
- There’s no one-size-fits-all solution to fasting with diabetes, and regardless of what type of diabetes you’re living with, you should always get the okay from your doctor or endocrinology specialist before attempting any intermittent fasting plan.
Intermittent fasting for diabetes
All that versatility we mentioned with respect to the “what” and “how” of intermittent fasting is also present in the “why”: the reasons people may try intermittent fasting can include everything from supporting specific health goals, like weight or body fat loss, to reducing grocery spending or establishing more sustainable eating habits.
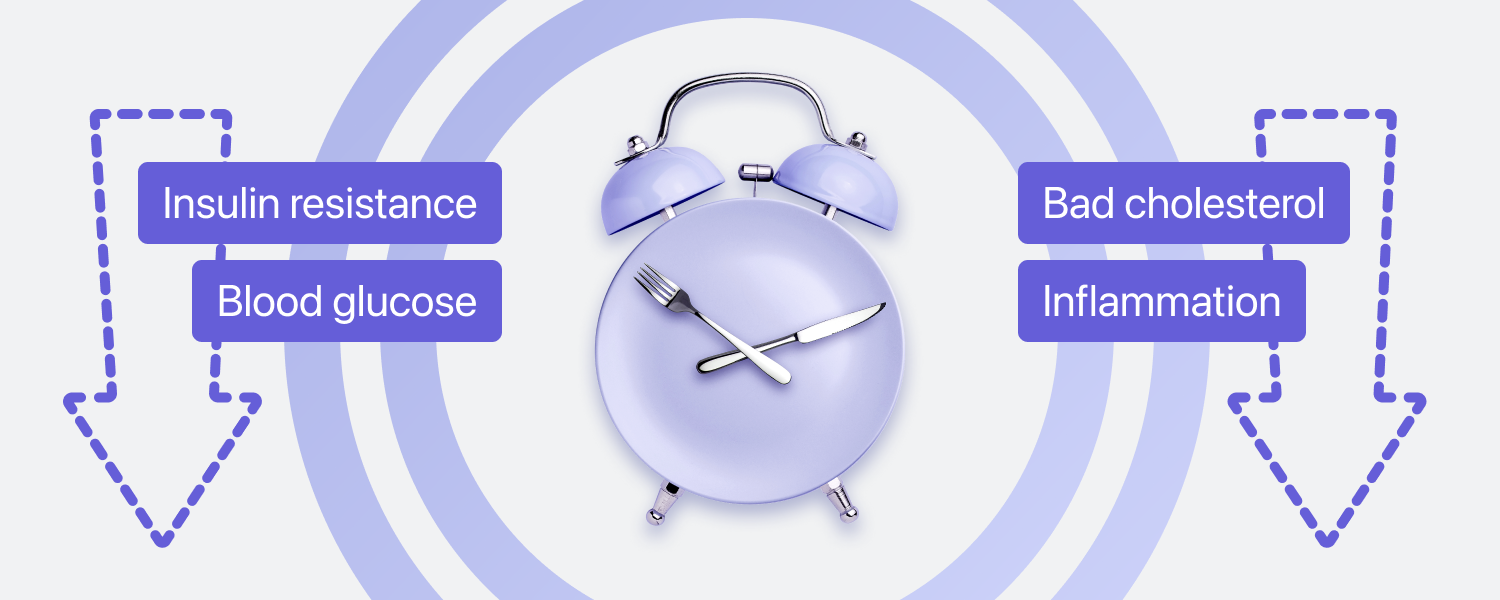
While motivations around fasting for diabetes can vary, too, there are a few common reasons someone with diabetes might consider this type of eating routine:
- It can be a helpful tool for weight management and for people living with obesity.[3,4]
- It may reduce insulin resistance and improve insulin sensitivity in people living with obesity.[5,6]
- It may decrease cholesterol and blood glucose (sugar) levels.[5,7]
- It may reduce inflammation, particularly in individuals living with overweight or obesity.[8]
In other words, intermittent fasting may generally improve your metabolic health. There is also some promising evidence that suggests intermittent fasting may support some people in putting their type 2 diabetes into remission, but it’s still early days, so we need more research before we can say that with confidence.
Let’s triple underline one phrase there: “type 2 diabetes.” Intermittent fasting can also be part of a supportive, health-promoting eating routine for someone with type 1 diabetes under certain conditions [9], but the research isn’t well established, and it’s not what we’re talking about here.
We’ll explore more details around the potential health benefits and risks of fasting with diabetes shortly, but as with any fasting routine, it’s important to remember that it may not be an effective, health-promoting choice for you and your goals.
So, if your doctor has deemed it safe, but you’re not sure if intermittent fasting is actually something you want to try, you can take our SIMPLE quiz to learn more about your options and get customized advice and support. You can think of it like this: if your doctor is your coach and playmaker, we’re the teammates who help you actually make it all happen!
What is intermittent fasting and how does it work?
Whatever style of intermittent fasting you try — and for whatever reasons — the process involves switching between periods of fasting and periods of eating on a regular schedule.
Different approaches require different periods and timelines of eating and fasting, and some also involve calorie restrictions. However, the fundamental concept is always the same: for a defined period, you take a complete break from eating.
And you can say goodbye to super restrictive meal plans: no foods are completely off the table because intermittent fasting is all about when not what you eat. You still want to give your body all the nutritious power-ups it needs, but you can also feed your soul that piece of cake it’s craving. (Though you may want to check out our guides on what to eat during intermittent fasting, what you can drink while fasting, and what breaks a fast to see what eating habits might mesh best with your personal goals!)
Wait, hold up.
What is this silver bullet of an eating routine? It sounds like magic.
No, you haven’t just found yourself in some fantastical show on The CW (sorry to everyone hoping for a meet-cute with a sexy vampire). It’s not magic — it’s science.
Imagine you just finished a meal. After you eat, your body starts turning food into helpful body stuff, like energy, fat, muscle, and brain power. Once it spends a few hours digesting and distributing everything, it’s happy to chill in what’s called a post-absorptive state for the next 8–12 hours.
After that internal R&R, your body then enters a fasted state. In this fasted state, your body is primed to burn fat instead of sugar to use as fuel. Think of it like dipping into your personal power reserves. (This process can affect some people living with diabetes differently, though, which we’ll explain in the next section!)
On your average day, you likely won’t go long enough without eating to trigger this state, so intermittent fasting is a straightforward way to initiate this natural body phase.
Want a bit more of a biology lesson with a healthy dose of history on the side? Take a look at our intermittent fasting for beginners guide.
How does intermittent fasting work for diabetes?
Since type 2 diabetes is often a lifestyle-related metabolic condition (as opposed to type 1 diabetes, which is hereditary), it affects how your body processes sugar.[10] Characterized by chronic inflammation, high levels of blood sugar, and decreased sensitivity to insulin, it can be helped through weight loss and improved insulin sensitivity to manage blood sugar levels.
Intermittent fasting can be used to do just that. When your body is in that fasted state, your insulin levels are lower, your body burns stored fat, and your blood glucose levels are more stable. Calorie restriction also improves insulin resistance.[11]
So basically, intermittent fasting can be your secret weapon for improving your diabetes management or slashing your chances of developing it in the first place.
And so far, the evidence stacks up: intermittent fasting (especially time-restricted eating approaches) can lead to weight loss and improvements in both blood sugar levels and insulin sensitivity [12], all of which are important in managing and preventing type 2 diabetes.
If you’re living with type 1 diabetes, or you’re living with type 2 diabetes and you’re on medication that lowers your blood sugar, intermittent fasting can hit differently, though. That’s because when your liver processes fat instead of sugar, it produces a fuel called ketones, which causes blood to become acidic and can lead to a life-threatening condition called diabetic ketoacidosis. That’s why working with your healthcare professional is super important if you’re playing matchmaker with diabetes and intermittent fasting.
Plus, more fasting or staying in that fasted state for longer doesn’t mean more benefits. Everyone has an optimal fasting window if fasting is appropriate for them, and you want to find what’s right for you and your unique body.
Is it the same for type 1 and type 2 diabetes?
As with any eating routine, the process and effects of intermittent fasting can vary from person to person. However, for people living with type 1 diabetes, or people taking blood sugar lowering medications for type 2 diabetes, the risk of extreme fluctuations in blood sugar levels can skyrocket with intermittent fasting — which basically can turn into a rollercoaster of hypoglycemia (blood sugar levels less than 4 mmol/L [13]) and hyperglycemia (blood sugar levels above 7 mmol/L before a meal and above 8.5 mmol/L two hours after a meal [14]).
That’s why it’s absolutely critical that you get support from your healthcare provider and build in even more blood sugar checks to make sure everything is stable. Even if you’re a thrill-seeker, your health is definitely not the place for risk-taking!
Recommended types of intermittent fasting schedules for diabetes
As long as your healthcare provider has approved your approach, there’s no right way or one way to do intermittent fasting — it’s all about finding what feels right to you. That means letting your body, nutritional needs, fasting goals, schedule, preferences, and lifestyle guide your methods.
That said, some approaches are generally easier to manage and might be a better starting point. Likewise, there are some approaches (like water fasting, OMAD, intermittent fasting 20:4, or eat stop eat) our experts don’t tend to recommend for people with diabetes unless you’re being very closely supervised. That’s because, generally speaking, fasts longer than 18 hours have the highest risk profile — not to mention it’s more difficult to maintain stable blood sugar.
While there are loads of different intermittent fasting plans out there, you can generally divide these plans into two categories: time-restricted eating and periodic fasting.
Time-restricted eating
If you’ve ever skipped breakfast or had an early dinner, chances are you’ve experienced a fast akin to a time-restricted eating plan. These protocols divide each day between “eating windows” (where you can eat as you normally would) and “fasting windows” (where you don’t consume anything other than zero-calorie drinks).
For example, you might choose to fast for 14 hours and eat during a 10-hour eating window (intermittent fasting 14:10) or fast for 16 hours and eat during an 8-hour window (intermittent fasting 16:8). You could even stretch that fasting window to 18 hours (intermittent fasting 18:6), although that can be a little tougher for blood sugar management.
You can also choose how to structure these different windows so they suit your preferences and daily schedule. Maybe that morning yogurt and granola is what helps you get out of bed. (Or maybe that’s the heavily caffeinated mocha on the side … either way, no need to miss out.)
We tend to recommend these types of plans — at least the 14:10 and 16:8 — for fasting beginners because they offer more freedom and flexibility with less routine change. Plus, shorter fasting windows can mean a reduced risk of side effects. For example, one study suggests that time-restricted eating may result in weight loss and improve insulin sensitivity without severe negative effects for people with type 2 diabetes or prediabetes.[12]
Periodic fasting
Unless you’re someone who does better with on / off routines, periodic fasting tends to be better for people who have had previous fasting success. Some of the more extreme forms involve going entirely without calories for an extended time (24+ hours), while others involve some days with significant calorie restriction (eating 500–600 calories, or roughly 25% of your usual daily intake) in lieu of being completely food-free.
Two of the most common periodic fasting methods include the 5:2 diet (eating normally for five days of the week and restricting calories for the other two) and alternate day fasting (alternating days of typical eating patterns with days of calorie restriction).
While some research suggests periodic fasting may lead to weight loss and substantial improvement in risk factors for diseases like type 2 diabetes [15], we still advocate for testing time-restricted eating approaches first since 500–600 calories is a very low amount and could introduce more health risks.
If you’re wondering which plan(s), if any, might work for you, you can always take our SIMPLE quiz. We’ve also got loads of tips and expert support on how to get started and stay motivated. But we can’t emphasize this enough, make sure to run everything by your doctor before actually trying anything, even if they already green-lit fasting in general!
Health risks and benefits of intermittent fasting with diabetes

So, you spoke to your doctor? Check.
And they approved a fasting plan that sounds like a good fit for you? Check.
Now what?
Unfortunately, what does or doesn’t happen next isn’t a guarantee. What works (or doesn’t) for your body may not have the same effect on someone else. Plus, while there is a lot of research on intermittent fasting in general and on intermittent fasting with prediabetes or type 2 diabetes [5,16], there isn’t a ton out there that focuses on intermittent fasting and type 1 diabetes.
We know it’s frustrating not having a universal, crystal clear answer to “Is fasting good for diabetes?” but we’ve rounded up the latest research on possible benefits and risks so you at least have an idea of what to expect. You can also check out our general intermittent fasting side effects guide.

Health benefits of intermittent fasting
Weight loss
For people living with type 2 diabetes, losing weight could send diabetes into remission. A significant amount of evidence supports that it can be an effective, safe method for weight loss and body fat loss [17,18], especially when paired with physical activity and strength training.[19] Some research also suggests intermittent fasting may actually be more effective for weight loss than calorie-restricted diets for people with type 2 diabetes.[17]
Reduced insulin resistance and improved insulin sensitivity
Particularly for people living with type 2 diabetes, obesity, and other metabolic conditions, intermittent fasting has been linked to reduced insulin resistance and improved insulin sensitivity.[5] It may also promote better blood sugar metabolism in general.[20]
Reduced inflammation
Systematic inflammation can contribute to a wide variety of health conditions, including heart disease and type 2 diabetes. Some studies have linked intermittent fasting to reducing inflammation [8], particularly for people living with type 2 diabetes or obesity.[21]
Decreased cholesterol
People living with diabetes have elevated blood sugar levels and thus may be more likely to have high cholesterol. There is some evidence to suggest intermittent fasting can help lower it for those living with type 2 diabetes.[5]
Health risks of intermittent fasting
Hyperglycemia and hypoglycemia
Fasting causes fluctuations in blood sugar levels, and people living with diabetes, especially those taking insulin or blood sugar lowering medications, are especially sensitive to these fluctuations. Situations where blood sugar levels drop too low (hypoglycemia [13]) or spike too high (hyperglycemia [14]) can be dangerous and even life-threatening.
Hormonal imbalance
Some research suggests that assigned-at-birth men and women may respond differently to intermittent fasting because it may decrease certain reproductive hormones while increasing or not affecting others.[22] For example, fasting may decrease androgens (like testosterone) and increase hormone-binding proteins that improve insulin sensitivity in women living with obesity and polycystic ovarian syndrome, but reductions in androgens may be detrimental to men. However, existing research is very limited and fails to explore the effects of fasting specifically on trans men and women and individuals currently on hormone replacement therapy.
Dehydration
During fasting, your body needs extra fluids to stay hydrated and maintain steady blood pressure, and changes to fluid intake can affect certain medications that people with diabetes may be taking.[23]
Should you try intermittent fasting if you are living with diabetes?
First and foremost, fasting with diabetes is not a time to resurrect your teenage rebellion phase — you should only try fasting if your doctor is on board and has signed off on a specific plan.
Once you have that permission slip, it’s about getting up close and personal with yourself. We’re talking “monitoring your blood sugar and symptoms like a hawk” close. Fasting affects everyone differently, and just because you’ve gotten permission to try it on doesn’t mean it’s the best fit for your body.
Who should avoid fasting?
People living with diabetes aren’t the only ones who should involve healthcare providers before making any decisions that may impact their health. You should also be particularly cautious about intermittent fasting if you:
- Have another medical condition;
- Are pregnant, breastfeeding, or trying to conceive;
- Have a history of or are currently diagnosed with either an eating disorder or disordered eating;
- Are under the age of 18, or 80 years old or more; or
- Are prescribed medication (for example, anti-hypertensives or any that need to be taken with food).
5 tips for intermittent fasting while having diabetes

We know we’re probably bordering broken record territory here, but we really can’t say it enough: before you start an intermittent fasting plan or make any adjustments to your eating habits, consult your healthcare professional. If they’ve given you the all clear, here are our experts’ top tips for intermittent fasting with diabetes.
- Monitor your blood sugar even more closely than usual. If you experience any symptoms of too high or too low blood sugar, break the fast immediately and check in with your doctor before trying the fast again.
- Focus on nutrient-dense foods with a low glycemic index during your eating windows. Eating ultra-processed or high-carb foods can spike your blood sugar. Prioritizing fiber, lean protein, fruits, and leafy vegetables will help keep your blood sugar more stable for longer.
- Drink lots of fluids. Staying hydrated is super important for any fast, so keep topping up that water bottle. (Coffee and tea without any cream or sugar are okay, and you can have one or two cans of diet soda, too.)
- Be prepared for some side effects. It’s common for intermittent fasting to cause some irritability, fatigue, headaches, and hunger at first. These feelings will pass after a week or two, but if you’re experiencing more severe, consistent, or longer-lasting symptoms, check in with your doctor.
- Enlist some support. It can be difficult to spot and react to hypoglycemic or hyperglycemic symptoms since you may become disoriented. Ensure your family, coworkers, or the people you’re with when you are fasting are aware of the signs and know how and where to seek help if you need it.
Tried all of the above and still feel like you’re not seeing the results you hoped for? In addition to reconvening with your doctor, you can troubleshoot with our “intermittent fasting not working” and “intermittent fasting mistakes” guides.
Simple’s expert opinion and final thoughts
Intermittent fasting can be helpful in managing diabetes and preventing it from occurring in the first place, but everyone responds to fasting differently, and it may not be a safe or health-promoting step for you. You should always consult your doctor and work with them to come up with an action plan before you put any fasting approaches to the test.
Ultimately, the best eating routine is the one that is right for you and your needs — and one that you can stick to. If your health provider has given you the go-ahead, you can take our SIMPLE quiz today to learn more about which intermittent fasting approach(es) might work best for you.
Frequently asked questions about intermittent fasting for diabetes
Can intermittent fasting help with diabetes?
Yes, intermittent fasting can help with diabetes, but it isn’t safe (or effective) for everyone. While intermittent fasting can help with weight loss, insulin sensitivity, and cardio-metabolic health, you should always consult your doctor before attempting any fasting routine.
How many hours should a person with diabetes fast?
There’s no magic number for how many hours a person with diabetes should fast; everyone is different, and everyone will likely have a different optimal fasting window. You should work with your doctor to find out what might work best for you, but we recommend avoiding fasting for longer than 16–18 hours if you’re living with diabetes.
Should someone with type 2 diabetes do intermittent fasting?
Intermittent fasting can be helpful in treating type 2 diabetes — and some early research suggests it may help send it into remission [24] — but not everyone with type 2 diabetes should do intermittent fasting. You should always consult your doctor first to find out if it’s a safe and potentially effective approach for your body.
What is the best intermittent fasting schedule for those with diabetes?
What intermittent fasting schedule is best for diabetes is based on your individual characteristics and circumstances. If you’re fasting for diabetes, speak with your healthcare provider about different options and which might be your perfect match.
Does fasting help lower blood sugar?
Fasting can help lower blood sugar. While decreased blood sugar levels can be helpful in treating type 2 diabetes, it can be dangerous if your blood sugar drops too low, so it’s important to keep a close eye on your levels.
- Borgundvaag E, Mak J, Kramer CK. Metabolic Impact of Intermittent Fasting in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis of Interventional Studies. J Clin Endocrinol Metab. 2021 Mar 8;106(3):902–11.
- Albosta M, Bakke J. Intermittent fasting: is there a role in the treatment of diabetes? A review of the literature and guide for primary care physicians. Clin Diabetes Endocrinol. 2021 Feb 3;7(1):3.
- Obermayer A, Tripolt NJ, Pferschy PN, Kojzar H, Aziz F, Müller A, et al. Efficacy and Safety of Intermittent Fasting in People With Insulin-Treated Type 2 Diabetes (INTERFAST-2)-A Randomized Controlled Trial. Diabetes Care. 2023 Feb 1;46(2):463–8.
- Welton S, Minty R, O’Driscoll T, Willms H, Poirier D, Madden S, et al. Intermittent fasting and weight loss: Systematic review. Can Fam Physician. 2020 Feb;66(2):117–25.
- Yuan X, Wang J, Yang S, Gao M, Cao L, Li X, et al. Effect of Intermittent Fasting Diet on Glucose and Lipid Metabolism and Insulin Resistance in Patients with Impaired Glucose and Lipid Metabolism: A Systematic Review and Meta-Analysis. Int J Endocrinol. 2022 Mar 24;2022:6999907.
- Che T, Yan C, Tian D, Zhang X, Liu X, Wu Z. Time-restricted feeding improves blood glucose and insulin sensitivity in overweight patients with type 2 diabetes: a randomised controlled trial. Nutr Metab . 2021 Oct 7;18(1):88.
- Meng H, Zhu L, Kord-Varkaneh H, O Santos H, Tinsley GM, Fu P. Effects of intermittent fasting and energy-restricted diets on lipid profile: A systematic review and meta-analysis. Nutrition. 2020 Sep;77:110801.
- Wang X, Yang Q, Liao Q, Li M, Zhang P, Santos HO, et al. Effects of intermittent fasting diets on plasma concentrations of inflammatory biomarkers: A systematic review and meta-analysis of randomized controlled trials. Nutrition. 2020 Aug 12;79-80:110974.
- Al-Ozairi E, El Samad A, Al Kandari J, Aldibbiat AM. Intermittent Fasting Could Be Safely Achieved in People With Type 1 Diabetes Undergoing Structured Education and Advanced Glucose Monitoring. Front Endocrinol . 2019 Dec 5;10:849.
- Zhang Y, Pan XF, Chen J, Xia L, Cao A, Zhang Y, et al. Combined lifestyle factors and risk of incident type 2 diabetes and prognosis among individuals with type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. Diabetologia. 2020 Jan;63(1):21–33.
- Napoleão A, Fernandes L, Miranda C, Marum AP. Effects of Calorie Restriction on Health Span and Insulin Resistance: Classic Calorie Restriction Diet vs. Ketosis-Inducing Diet. Nutrients [Internet]. 2021 Apr 15;13(4).
- Lin X, Guan Y, Wu G, Huang J, Wang S. Time-restricted eating for patients with diabetes and prediabetes: A systematic review. Front Nutr. 2022 Nov 3;9:1025919.
- American Diabetes Association. Hypoglycemia (low blood glucose) [Internet]. [cited 2023 May 24].
- American Diabetes Association. Hyperglycemia (high blood glucose) [Internet]. [cited 2023 May 24].
- Cui Y, Cai T, Zhou Z, Mu Y, Lu Y, Gao Z, et al. Health Effects of Alternate-Day Fasting in Adults: A Systematic Review and Meta-Analysis. Front Nutr. 2020 Nov 24;7:586036.
- Sharma SK, Mudgal SK, Kalra S, Gaur R, Agarwal R. Effect of Intermittent Fasting on Glycaemic Control in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Endocrinology. 2023;19(1).
- Wang X, Li Q, Liu Y, Jiang H, Chen W. Intermittent fasting versus continuous energy-restricted diet for patients with type 2 diabetes mellitus and metabolic syndrome for glycemic control: A systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract. 2021 Sep;179:109003.
- Carter S, Clifton PM, Keogh JB. The effect of intermittent compared with continuous energy restriction on glycaemic control in patients with type 2 diabetes: 24-month follow-up of a randomised noninferiority trial. Diabetes Res Clin Pract. 2019 May;151:11–9.
- Abeyasekera KN. Benefits of Intermittent Fasting: A Systematic Review of Randomized Clinical Trials. Physician Assistant Studies. Student Articles. 12. 2020.
- Teong XT, Liu K, Vincent AD, Bensalem J, Liu B, Hattersley KJ, et al. Intermittent fasting plus early time-restricted eating versus calorie restriction and standard care in adults at risk of type 2 diabetes: a randomized controlled trial. Nat Med. 2023 Apr;29(4):963–72.
- Oueslati I, Kardi A, Boukhayatia F, Hammami B, Cheikh M, Romdhane NB, et al. Impact of Ramadan intermittent fasting on metabolic and inflammatory profiles in type 2 diabetic patients. J Diabetes Metab Disord. 2022 Jun;21(1):751–8.
- Cienfuegos S, Corapi S, Gabel K, Ezpeleta M, Kalam F, Lin S, et al. Effect of Intermittent Fasting on Reproductive Hormone Levels in Females and Males: A Review of Human Trials. Nutrients [Internet]. 2022 Jun 3;14(11).
- Grajower MM, Horne BD. Clinical Management of Intermittent Fasting in Patients with Diabetes Mellitus. Nutrients [Internet]. 2019 Apr 18;11(4).
- Yang X, Zhou J, Shao H, Huang B, Kang X, Wu R, et al. Effect of an Intermittent Calorie-restricted Diet on Type 2 Diabetes Remission: A Randomized Controlled Trial. J Clin Endocrinol Metab. 2023 May 17;108(6):1415–24.
