Intermittent fasting and women’s hormones: how they interact

To date, thousands of women have used the Simple app to support their intermittent fasting journey. Whether it’s losing weight, improving their health, having more energy, or “all of the above and more,” Simple’s female users have enjoyed many benefits from intermittent fasting — a dietary approach that involves alternating between periods of eating and fasting.

But what about fasting’s impact on women’s hormones? Is intermittent fasting bad for women’s hormones … or safe enough to try?
How does intermittent fasting affect female hormones, particularly for women looking to lose weight, transform their bodies, and enhance their health through this dietary practice?
In this article, we’ll delve into the intricacies of intermittent fasting and explore its interactions with women’s hormones.
Navigating intermittent fasting as a woman can be intricate. Don’t go at it alone! Simple’s nutrition assistant Avo™ is here to answer your questions and provide tailored recipe ideas. Plus, stay on track with hydration reminders and an intuitive food journal. Dive deep into your health journey and get insights with personalized feedback. Take the Simple quiz to start your wellness journey.
Does fasting affect hormones?
Let’s start with a basic overview of how intermittent fasting can affect hormones in general before looking at how fasting affects women’s hormones in particular.
(For more on the basics of fasting, check out intermittent fasting for beginners.)
Hormones are strongly influenced by intermittent fasting.
Taking a break from eating for 8–10 hours or more (for instance, like Simple’s time-restricted eating routine, where people might fast for 12 to 18 hours with an eating window of 6 to 12 hours) can affect the levels of hormones such as:[1]
- growth hormone, which is involved in growth, development, and repair
- insulin, which helps us manage blood sugar and transport it into cells, but also helps signal the body to break down fat when its levels are low (such as when we’re fasting)
- leptin, which helps sense how much energy we have and manages our appetite
- glucagon, which helps break down stored fuel in the liver
- adrenaline, which also helps mobilize stored fat for energy and often gives people an “energy boost” while fasting
- adiponectin, which also helps break down fat so we can burn it
- cortisol, which is involved in our stress response
OK, so you get the idea that fasting affects many hormones, which can help explain why intermittent fasting may help us improve our health and lose weight.
But what about female bodies specifically — how do intermittent fasting and female hormones interact?
How does intermittent fasting affect women’s hormones?
Importantly, the hormonal effects of intermittent fasting can differ between women and across an individual woman’s lifetime.
So the short version of this section is: it depends.
Here, we’ll explore how intermittent fasting can influence women’s hormones, particularly reproductive hormones.
(For more on other women’s health topics, check out our articles on “Intermittent Fasting for Women” and “Intermittent Fasting for Women Over 50.”)
Reproductive hormones are mainly produced in the ovaries or the brain. However, some (like DHEA) are also produced in the adrenal glands atop the kidneys and by adipose (fat) tissue — which will be important later, so stay tuned!
Estrogen
Estrogen (estradiol) is one of the main hormones that regulate reproduction in women between puberty and menopause. It has many roles in the body, such as:[2]
- breast development and health
- ovarian function
- uterine development and health
- vaginal health
- bone development and health
- cardiovascular health
- brain health
When estrogen levels fall, it can trigger symptoms of menopause, like hot flashes.[3]
On the other hand, intermittent fasting could potentially be part of preventing some types of reproductive cancers linked to too-high estrogen, such as breast cancer.[4]
However, newer research showed that eight weeks of intermittent fasting did not lower estrogen levels.[5]
Clearly, the relationship between intermittent fasting and estrogen levels remains complex; further research is crucial to determine how exactly they interact with one another.
Progesterone
Progesterone helps prepare the lining of the uterus to receive a potentially fertilized egg for pregnancy. However, like estrogen, it also has many other jobs in the body, such as:[6]
- bone health
- brain health [7]
Follicle-stimulating hormone (FSH) and luteinizing hormone (LH)
These are hormones produced by the pituitary gland in the brain. They work together to help regulate the menstrual cycle.[8,9]
Research on intermittent fasting using a 16:8 routine (16 hours of fasting and an 8-hour eating window) showed no effect on FSH and LH, which is good news.[1,10]
Androgens: testosterone, androstenedione, and DHEA
Yes! Women have testosterone, too! Androgens play a role in women’s sexual response and can be aromatized (aka converted) to estrogen.[9,11]
While the ovaries produce some androgens, the adrenals produce most of these types of hormones. For instance, DHEA is produced by the adrenal glands and is an important hormone for women going through the menopause transition.[12]
Many women with polycystic ovary syndrome (PCOS) produce too many androgens, which then inhibit proper ovulation and egg release.[13,14] These women also often have high circulating insulin levels, which can lead to insulin resistance.[15]
Intermittent fasting may be helpful for women with PCOS, as it can support weight loss along with possibly lowering high androgen and insulin levels.[1] (If this is you, consult with your healthcare provider before making any dietary changes, as PCOS often requires medical support.)
Sex hormone binding globulin (SHBG)
This isn’t a hormone but rather a protein that helps carry hormones around the body. Levels of SHBG help influence how much of a given hormone is available for cells to use.
Some reproductive disorders like PCOS are linked to low levels of SHBG. Intermittent fasting appears to increase SHBG, which may help some women.[1] More research is needed to further back this up, but the findings are extremely exciting.
Gut microbiome
OK, this one really isn’t a hormone … but it may affect levels of sex hormones, too. Our gut microbiome is the collection of friendly microorganisms that live in our digestive tract.
Fun fact: these little critters help regulate sex hormone levels as well. Since intermittent fasting has been shown to have positive effects on our gut microbiome,[16] we might also see positive effects on sex hormones.
Feeding your gut microbes is one reason we recommend eating a higher-fiber diet. In your Simple app, you’ll find a personalized nutrition score that includes fiber. Take the Simple quiz to get started today!
Intermittent fasting during different female hormonal stages

Women go through various hormonal stages in their lives, including puberty, the menstrual years, (potentially) pregnancy, menopause, and beyond.
Here’s how intermittent fasting can interact with these different stages.
Puberty and early adult years
At puberty, menarche (the first menstrual period) occurs, and girls go through several years of development before becoming mature women. They’ll have much higher sex hormone levels than during childhood, including a temporary increase in androgens.
During adolescence and early adulthood, as girls are growing, developing, and working towards peak bone density in their 20s, it’s essential for them to ensure they are meeting their nutritional needs.
At Simple, we do not recommend fasting for anyone younger than 18, or anyone who is 80 years old or more.
Reproductive years
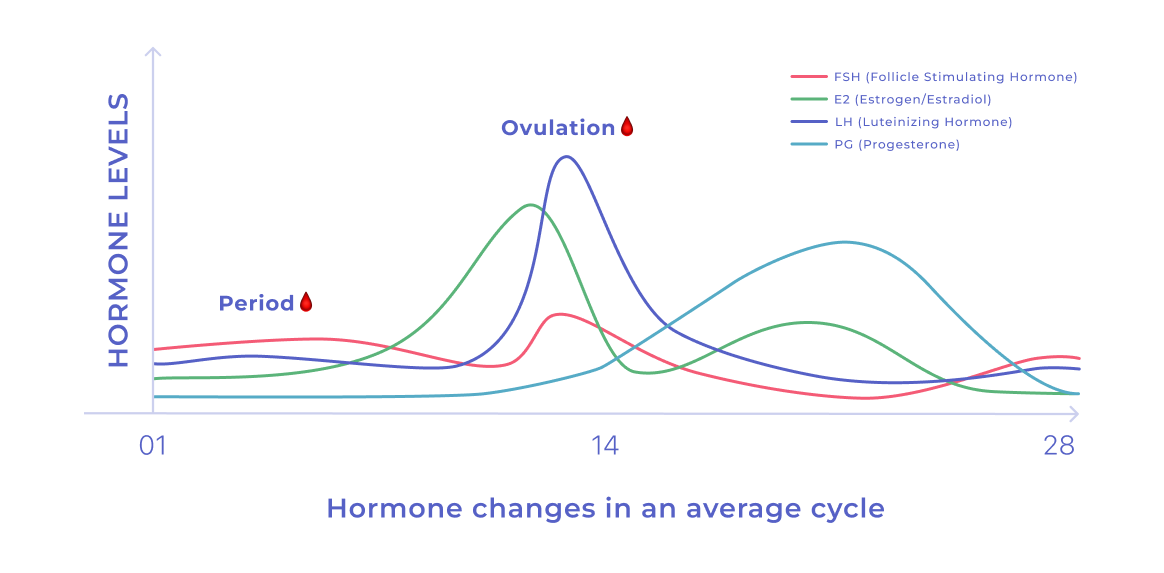
For women with uteruses, the time between menarche and menopause marks the reproductive years. Whether they choose to actually reproduce or not, their bodies will cycle through a menstrual cycle with menstrual periods approximately once a month. This cycle is organized by hormones such as estradiol, progesterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH).[17]
The menstrual cycle officially starts on the first day of a woman’s period. During the first two weeks, estrogen levels slowly rise as women approach ovulation (or the release of an egg from the ovary).
Around ovulation, estrogen peaks, along with FSH and LH. This combined activity results in the ovary releasing an egg from the ovarian follicle.
Once freed, the egg travels down the fallopian tube to the uterus. Meanwhile, the empty follicle begins to secrete progesterone, which helps prepare the uterine lining, just in case the egg is fertilized. If the egg isn’t fertilized, the uterus sheds its lining, and the cycle begins again.
All of this depends on having the right levels of reproductive hormones.
Evidence suggests that for healthy women who don’t restrict their calories stringently, time-restricted eating generally does not harm normal menstrual cycles.[1]
That said, women who are focused on fertility and trying to conceive should consult with a healthcare professional before implementing intermittent fasting to ensure it aligns with their reproductive goals.
Pregnancy and postpartum
Intermittent fasting while pregnant or breastfeeding? That’s a big NO from us.
Mom and baby need plenty of energy and nutrients, so we do not recommend intermittent fasting during this phase.
Perimenopause, menopause, and beyond
Perimenopause — the several years of transition before the final period of menopause — is marked by hormonal fluctuations that can bring many unwanted symptoms for women in their 40s and early 50s.
These symptoms emerge largely from declining estrogen and can include hot flashes, night sweats, irregular menstrual cycles, mood swings, vaginal dryness, decreased libido, fatigue, and bone density loss. Women may notice weight gain, especially around their middle.[18]
These symptoms can also occur after menopause (i.e., 12 months after the final menstrual period) and for women who have had surgical menopause and are not supplementing additional estrogen.
While intermittent fasting can’t necessarily help directly with perimenopausal or menopausal symptoms, it can support weight management.[19]
After menopause, with much less estrogen and progesterone, women’s risk of many chronic health problems — such as cardiovascular disease or high blood pressure — goes up dramatically.[20,21]
By helping support overall metabolic health, intermittent fasting may also lower some post-menopausal women’s risk of these types of health problems.
However, we don’t encourage fasting for any women over the age of 80. (Here’s a handy intermittent fasting by age chart that can help guide you.)
Does fasting balance hormones?
Many women wonder whether intermittent fasting could help balance their hormones. And many have tried intermittent fasting specifically for hormone balance.
There’s good and bad news here.
Bad news first: You can’t “balance” hormones.
Hormones and their interactions are very complex, and hormones are often released in pulses. (Think of one of those lawn sprinklers that goes blup-blup-blup, releasing the water in little bursts rather than a hose with a steady, constant stream.)
So, in simple terms, hormones are always up to stuff and talking to each other (chemically, at least), which is always changing from moment to moment.
Women who menstruate will also have natural and normal ups and downs in key hormones across their cycle.
However, this doesn’t mean that intermittent fasting isn’t working. Because …
The good news is that fasting may improve hormonal health for some people by helping hormones live within their optimal ranges.
This can happen, for example, in the following ways:
- For some women, intermittent fasting may help normalize insulin levels, which can help decrease insulin resistance and, in turn, increase SHBG levels.[1]
- When women lose weight, it can affect the amount and type of hormones their adipose (fat) tissue produces. Women with high body fat may have a lot of excess hormones produced. But losing some of this fat may improve overall health as there is less adipose tissue to produce those hormones. This can help adjust hormone levels to normal ranges.[22]
So, does fasting balance hormones? No, but it may help improve women’s hormonal health in other ways.
Intermittent fasting’s impact on men vs. women
While the fundamentals of intermittent fasting are similar for both men and women, there are some important sex differences.[1]
- “Defend the fort” response: Women’s bodies tend to be more sensitive to having less energy (i.e., calories) available. They respond faster and more aggressively to a situation that signals potential starvation — which can include dialing down metabolic rate via the thyroid or inhibiting reproductive functions (like having a menstrual cycle).[23] So, does intermittent fasting in general slow metabolism? Luckily, there is evidence that intermittent fasting may outperform conventional “diets” for preventing this metabolism slowdown.
- More appetite: As part of the “defend the fort” response, women’s appetite hormones may go up faster than men’s as the body tries to maintain its energy stores.[24] This is one of the more common, but manageable, side effects of fasting.
- Weight loss: Both men and women can lose weight with intermittent fasting, but the rate and extent of weight loss may vary due to hormonal differences.[1]
Safety tips for women practicing intermittent fasting

If you’re a woman considering intermittent fasting, here are some safety tips to keep in mind.
- Consult a healthcare provider before making any major dietary or lifestyle changes — especially if you have underlying health conditions or are pregnant.
- Don’t fast aggressively or restrict food stringently. Both of these will likely affect hormonal health, especially long term. While moderate time-restricted eating (again, like a 12- to 8-hour eating window combined with a 12- to 16-hour fasting period) doesn’t seem to disrupt hormones in healthy women, more extensive fasting may cause problems.
- Listen to your body: This includes observing changes in normal menstruation (if you have cycles) or in symptoms of perimenopause / menopause (if you’re at that stage). And, of course, if you feel extremely hungry, dizzy, or uncomfortable, consider adjusting your fasting routine or seeking guidance from a healthcare provider.
- Nourish yourself: When you do eat, focus on nutrient-rich foods to ensure you’re meeting your nutritional needs. Our Simple Nutrition Scores can help!
- Avoid extreme fasting: Look for moderate, sustainable lifestyle changes rather than aggressive measures. Slow and steady is the name of the game! So, no to all-day fasts or water fasts.
Many women do notice more belly fat and body weight gain around the menopausal transition as hormone levels change.
Intermittent fasting may help reduce visceral fat, including belly fat, which can positively impact hormonal balance.[19,25] However, results may vary among individual women.
Low estrogen levels in women can lead to symptoms such as hot flashes, night sweats, irregular menstrual cycles, mood swings, vaginal dryness, decreased libido, fatigue, and bone density loss.
These symptoms often occur during menopause but can also result from other hormonal imbalances or medical conditions. If you have any concerns about low estrogen or any other health issue, please consult your doctor.
There isn’t really one. Your best bet is to eat a nutrient-rich diet. Simple can help with personalized feedback on your diet via our Nutrition Scores feature. (And check out our helpful guide on what to eat during intermittent fasting.)
No, and we don’t recommend water fasting. No evidence supports it, it doesn’t help us in any way, and the risks are significant.
In fact, not drinking enough water is one of the most common intermittent fasting mistakes — and water is a perfect drink while fasting.
You can’t really “reset” your hormones.
But you can improve your overall health and well-being with wise lifestyle choices that may include intermittent fasting (along with a nutrient-rich diet, regular exercise, sleep, and stress management).
Any hormonal changes through diet and lifestyle adjustments will take time and vary widely between individual women.
Key hormones that affect women’s metabolism include insulin, appetite hormones like leptin and ghrelin, stress hormones like cortisol, thyroid hormones, and sex hormones like estrogen and progesterone.[26]

- Cienfuegos S, Corapi S, Gabel K, Ezpeleta M, Kalam F, Lin S, et al. Effect of Intermittent Fasting on Reproductive Hormone Levels in Females and Males: A Review of Human Trials. Nutrients [Internet]. 2022 Jun 3;14(11).
- Prior JC. Women’s reproductive system as balanced estradiol and progesterone actions—A revolutionary, paradigm-shifting concept in women’s health. Drug Discov Today Dis Models. 2020 Dec 1;32:31–40.
- Lizcano F, Guzmán G. Estrogen Deficiency and the Origin of Obesity during Menopause. Biomed Res Int. 2014 Mar 6;2014:757461.
- Endogenous Hormones and Breast Cancer Collaborative Group, Key TJ, Appleby PN, Reeves GK, Roddam AW, Helzlsouer KJ, et al. Circulating sex hormones and breast cancer risk factors in postmenopausal women: reanalysis of 13 studies. Br J Cancer. 2011 Aug 23;105(5):709–22.
- Kalam F, Akasheh RT, Cienfuegos S, Ankireddy A, Gabel K, Ezpeleta M, et al. Effect of time-restricted eating on sex hormone levels in premenopausal and postmenopausal females. Obesity . 2023 Feb;31 Suppl 1(Suppl 1):57–62.
- Cable JK, Grider MH. Physiology, Progesterone. StatPearls Publishing; 2023.
- Zubeldia-Brenner L, Roselli CE, Recabarren SE, Gonzalez Deniselle MC, Lara HE. Developmental and Functional Effects of Steroid Hormones on the Neuroendocrine Axis and Spinal Cord. J Neuroendocrinol [Internet]. 2016 Jul;28(7).
- Orlowski M, Sarao MS. Physiology, Follicle Stimulating Hormone. StatPearls Publishing; 2023.
- Nedresky D, Singh G. Physiology, Luteinizing Hormone. StatPearls Publishing; 2022.
- Li C, Xing C, Zhang J, Zhao H, Shi W, He B. Eight-hour time-restricted feeding improves endocrine and metabolic profiles in women with anovulatory polycystic ovary syndrome. J Transl Med. 2021 Apr 13;19(1):148.
- Nassar GN, Leslie SW. Physiology, Testosterone. StatPearls Publishing; 2023.
- Dutt M, Wehrle CJ, Jialal I. Physiology, Adrenal Gland. StatPearls Publishing; 2023.
- Cussen L, McDonnell T, Bennett G, Thompson CJ, Sherlock M, O’Reilly MW. Approach to androgen excess in women: Clinical and biochemical insights. Clin Endocrinol . 2022 Aug;97(2):174–86.
- Xu Y, Qiao J. Association of Insulin Resistance and Elevated Androgen Levels with Polycystic Ovarian Syndrome (PCOS): A Review of Literature. J Healthc Eng. 2022 Mar 21;2022:9240569.
- Zhao H, Zhang J, Cheng X, Nie X, He B. Insulin resistance in polycystic ovary syndrome across various tissues: an updated review of pathogenesis, evaluation, and treatment. J Ovarian Res. 2023 Jan 11;16(1):9.
- Mohr AE, Gumpricht E, Sears DD, Sweazea KL. Recent advances and health implications of dietary fasting regimens on the gut microbiome. Am J Physiol Gastrointest Liver Physiol. 2021 May 1;320(5):G847–63.
- Lacroix AE, Gondal H, Shumway KR, Langaker MD. Physiology, Menarche. StatPearls Publishing; 2023.
- Santoro N. Perimenopause: From Research to Practice. J Womens Health . 2016 Apr;25(4):332–9.
- Welton S, Minty R, O’Driscoll T, Willms H, Poirier D, Madden S, et al. Intermittent fasting and weight loss: Systematic review. Can Fam Physician. 2020 Feb;66(2):117–25.
- Mehta JM, Manson JE. The menopausal transition period and cardiovascular risk. Nat Rev Cardiol [Internet]. 2023 Sep 26.
- Raman V, Kose V, Somalwar S, Dwidmuthe KS, Rao S. Prevalence of Metabolic Syndrome and Its Association With Menopausal Symptoms in Post-Menopausal Women: A Scoping Review. Cureus. 2023 May;15(5):e39069.
- Ylli D, Sidhu S, Parikh T, Burman KD. Endocrine Changes in Obesity. MDText.com, Inc.; 2022.
- Wu BN, O’Sullivan AJ. Sex differences in energy metabolism need to be considered with lifestyle modifications in humans. J Nutr Metab. 2011 Jun 6;2011:391809.
- Vigil P, Meléndez J, Petkovic G, Del Río JP. The importance of estradiol for body weight regulation in women. Front Endocrinol . 2022 Nov 7;13:951186.
- Rosenberg J, Jacob J, Desai P, Park J, Donovan L, Kim JY. Incretin Hormones: Pathophysiological Risk Factors and Potential Targets for Type 2 Diabetes. J Obes Metab Syndr. 2021 Sep 30;30(3):233–47.
- Schwarz NA, Rigby BR, La Bounty P, Shelmadine B, Bowden RG. A review of weight control strategies and their effects on the regulation of hormonal balance. J Nutr Metab. 2011 Jul 28;2011:237932.
